- Health Aether
- Posts
- The Liver-Bile-Thyroid Axis is the Protector of your Microbiome
The Liver-Bile-Thyroid Axis is the Protector of your Microbiome
How These Three Systems Impact Your Gut Health - And How to Fix Them
The Liver-Bile-Thyroid Axis is the protector of your microbiome. These three systems are whats holding the glue together to allow your gut & microbiome to thrive. A breakdown of one of these organ systems leads to a breakdown of all of them (Systems Theory).
Theory of Constraints proposes the idea that the weakest link in a system is the bottleneck for the whole. In terms of todays topic: Think of low thyroid functioning impacting the liver, hence bile flow, hence any downstream event.
The consequence: Gut Disease
SIBO
GERD
IBS/ IBD
Leaky Gut
Constipation
Ulcerative Colitis
And I have to witness this myself:
After a setback in my own healing journey, I considered bloodwork. Rightly so, as the blood work showed that this axis is bottlenecking the regeneration of my gut, microbiome & detoxification abilities.
So I set out a quest to improve these areas & in todays newsletter edition, I share all of the theory, practices & lifestyle improvements you can implement to improve this critical piece.
Discover the 3-part plan I use to regenerate the functioning of this axis.
Let’s dive in!
The liver: At the crossroads of gut & the body
The liver is the largest organ in our body and a metabolic powerhouse. Rightfully so, as its jobs are very widely spread.
Its roles include:
Glucose Metabolism
Protein Metabolism
Lipid Metabolism
Immune Functioning
Storing Function
Detoxification
The liver is at the crossroads of our gut & body, as it is the protector of our systemic blood circulation & hence body. See, the gut is a (rather) isolated system within us, as the gut barrier serves as a gatekeeper to what can enter our body & what cannot.
But even in healthy people, this barrier is not sealed completely, so there are always slow drips of toxins entering our body. In low amounts this is no problem as the liver is here to protect us.
Toxins include a wide variety of things:
Heavy metals
Endotoxins
Mycotoxins
Xenobiotics
Pesticides
Herbicides
Medications
Xenoestrogens
Especially endotoxins are important in later discussions.
These are lipopolysaccharides derived from gram-negative (“bad”) bacteria within our gut. If they feed on our food or die, they release LPS which can enter our bloodstream.
In the case of a healthy liver & gut, this is no problem at all. A tight sealing won’t let them pass and if that is the case, a healthy liver will detoxify them.
But a breakdown of a healthy gut microbiota leads to Leaky Gut, accompanied by dysbiosis, leading to increasing levels of LPS in the bloodstream, which leads to excessive inflammation.
And as you know, this is the worst enemy there is.

Now back to the liver talk. Supporting the liver is of utmost importance, so that we can lower inflammation & start addressing toxin overload, which is very, very common in this polluted world.
For this, we need some more insights into how liver detoxification works.
How does the liver metabolize toxins?
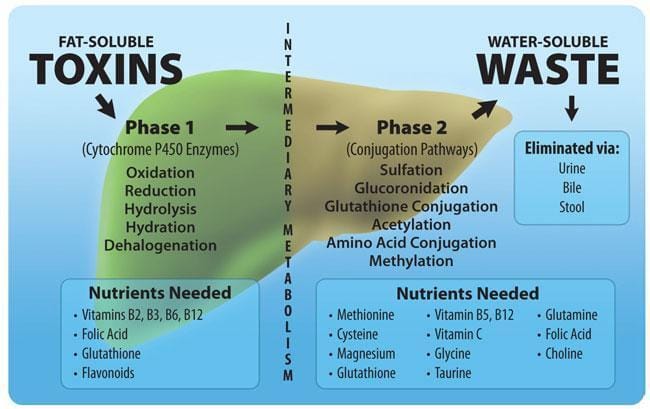
There are three phases to liver detoxification:
Phase1: Cyp450 enzymes metabolize fat-soluble toxins
Phase 2: Conjugation of these intermediates
Phase3: Excretion through bile, feces, urine
Like a conveyor belt, these three work in tandem to metabolize & excrete toxins. But just like a conveyor belt, a bottleneck along the journey leads to overflow of the system at one point, halting the whole process while possibly increasing inflammation.
Phase 1 detoxification is mainly ruled by an enzyme class called CYP450 enzymes. These heme based enzymes are very, very important in all sorts of detoxification, from mycotoxins to hormones.
Although we can find them everywhere, their highest expression is in the liver. For them to work efficiently, we need the right micronutrients to support NADPH & FAD/FMN metabolism (B1,B2,B3), mitochondrial efficiency to create heme (iron-copper dynamics), oxygen tensions & electron density.
Here is a simple overview their metabolism:
The toxin binds to its respective CYP enzyme
NADPH donates electrons to harness the reaction
The iron (found in heme) is turned into Fe2+
Oxygen binds to the iron (a bit like hemoglobin)
Another electron is needed
CYP enzyme transformation (can go many ways)

A problem occurs if this intermediate is even more toxic than its predecessor. This is common for mycotoxins, e.g. Aflatoxin B1 or other ones. Hence why between phase 1 & 2, we need antioxidants to keep ourselves protected if phase 2 cannot yet hold onto these intermediates.
Antioxidants are:
Vitamin C
Vitamin E
GSH
SODs
Melanin
Phase 2 conjugation is step where certain metabolites are attached to the aforementioned toxin, increasing their water-solubility for them to be excreted through various pathways.
Conjugation reactions involve the following:
Sulfation
Methylation
Glucoronidation
Glutathione Conjugation
Amino Acid Conjucation
Acetylation
Let’s get through them all, step by step & how we can optimize each of them.
Sulfation is a process where a sulfate group is added to the compound. It relies on good sulfate metabolism, with PAPS as the end product or sulfate carrier.
Sulfate availability is a real problem in todays world, due to a lack of sunshine. Dr. Stephanie Seneff proposes that under UV light, eNOS (an enzyme normally producing NO) liberates sulfate.
On the other hand, we have common micronutrient deficiencies on top of that:
B1
B6
Zinc
Molybdenum
These are the most important in terms of this pathway.

Methylation refers to a reaction where a methyl group (CH3) is attached to a molecule. As methylation is a hefty, long process, I want to refer to this newsletter here, where you learn how to optimize it the right way.
Glucoronidation is a process driven by UGT enzymes, taking UDP-glucoronic acid and transfer the latter onto a molecule. In my opinion this is an underrated detoxification pathway which we should optimize for as mycotoxins are known to be detoxified through this pathway.
Glutathione conjugation uses the glutathione redox system to metabolize toxins. The status of reduced glutathione (electron dense) is a very important redox indicator.
Redox is the state of the cell, where reduced is a state where electrons are plentiful and oxidized is a state of positive charge overload/ electron lack.

As you can see in this image, the whole antioxidant system is a web of systems integrated into systems. A bottleneck in one of those may break the other.
I wanna mention that Melanin, Melatonin or Nrf2, which are either directly acting as an antioxidant (Melanin, Melatonin) or are up regulating respective genes (Nrf2, Melatonin).
We will get into the “how to optimize” right after phase 3 explanation.
Amino acid conjugation is driven by, you guessed it, availability of certain amino acids. I wanna emphasize the role of taurine, glycine, cysteine, glutamine as these are all very important and often times lacking in modern food web.
Now, what happens when we got the toxins metabolized? Right, they have to go somewhere. The three main pathways the liver uses are:
Urine (through kidneys)
Bile (large, fat soluble molecules)
Feces (smaller molecules)
Yes, we have sweating & our expiration, but we will neglect them in this context.
Optimizing for phase 3 is done by optimizing hydration & electrolyte balance (kidneys), improving liver function & inflammation (bile) and getting at least 1 bowl movement per day, by optimizing gut dysbiosis & vagus nerve tone.
Here is an overview:
How are we detoxifying?
We have to understand that the right order is of utmost importance. For example, if we start upping the Phase 1 pathways, while having severe issues with Phase 3, we will have stuck toxins within our bile & feces.
Enterohepatic recirculation will then lead to a re-uptake of said toxins (through the so called portal vein). This increases inflammation & metabolic burden onto your liver.
So, we wanna optimize like this:
Phase 3 = Phase 2 > Phase 1
The latter is focused on, after we got the first two right. If you have severe issues with constipation, Phase 3 is even more important in earlier steps.
I want to give you a short list of the optimizing levers for each of them:
Phase 3:
Drinking 2-3l a day
Add electrolytes to every drink (Potassium!)
Vagal Stimulation (read here)
Asses for dysbiosis & leaky gut
Psoas & Lymph massages
Pomegranate/ Vitamin C/ Bitters/ Holy Basil/ Ginger/ Milk thistle
Magnesium Citrate/ Oxide, Senna, Cascara Sagrada
Phase 2:
We put a special emphasis on the pathways of glutathione, glucoronidation & sulfation, as I deem them to be very important & often dysfunctional:
For them to work, we will need a good diet to start with.

From that basis, we can build upon important nutrients to focus on.
Glutathione:
NAC/ Glycine/ Glutamine (fish, broths, supplements)
Vit E (Red Palm Oil)
Vit C (Fruit)
Manganese/ Selenium/ Zinc through organs & meat
Grounding to improve electron flow
Sulforaphane
Building up the melanin & melatonin through respecting circadian practices
Sulfation:
Sun, sun, sun
Vitamin B1
Molybdenum (might be worth as a supplement)
Zinc
B6
CoQ10
Glucoronidation:
Cruciferious vegetables (well cooked, in animal fat)
Citrus fruit of any form
Get on top of SIBO & any dysbiosis (due to ß-Glucoronidase enzyme)
Quercetin, Curcumin, Coffee, Green Tea
Work on high cortisol (breathing, trauma, stress)
Work on these (in company with thyroid & bile) for 4-8 weeks. We gotta get this phase firing.
For Cyp450, we first and foremost need very high amounts of B1, B2 & B3, as pre cursors for the reducing agents (NADPH & FAD). For these we also need superb magnesium, molybdenum, selenium, zinc & Vitamin B6 status.
As you have seen, these enzymes use oxygen for their reactions, but many of us are pseudohypoxic (= lacking oxygen within their cells). To combat this focus on iron-copper dynamics (here) and get into natures hyperbaric oxygen chamber.
This term was coined by a fellow of mine, Jack Schroder. We utilize mother nature to improve oxygen uptake into our cells, while increasing the amount of it used in ATP synthesis & molecular reactions.
The recipe is as follows:
Grounding: increases electron flow (anti-inflammatory) while improving “Zeta potential”. It is a fancy word of saying: my RBCs won’t clot as much, hence improved blood flow. This process gives substrate to our mitochondria. Also the electrons can actually change the redox state of iron & copper towards the ones we need.
Red light (preferably from the sun): this charge separates water within our cells & blood vessels, further improving blood flow and hence oxygen delivery to tissue. Red light improves mitochondrial energy production as it is a substrate for complexes 4 & 5. Last but not least, it creates singlet oxygen which then can enter any reaction more efficiently.
CO2 retention: increasing CO2 will lead to better oxygen usage, as it improves the binding properties of hemoglobin, letting loose of oxygen when it needs to. Buteyko Breathing is good here.
All in all, this is how you will improve CYP enzymes even further, as you hopefully focused on nutrients before. It might be worth to look into genes here to adjust dietary intake of micronutrients.
The liver-bile-gut link
When talking about liver metabolism, I left bile out of the discussion, though it is of utmost importance when we talk about the gut & metabolism. But first the basics.
Bile is synthesized in the liver via two ways: the classical pathway & the alternative pathway. Without going to deep, I wanna mention the following: Cholesterol & CYP7A1
Cholesterol is the backbone of every bile acid. Without it, there is no sufficient synthesis. Thats somewhat ironic, as one of the main functions of bile is to take up cholesterol in the gut. A vicious cycle is created if bile is low.
CYP7A1 is the bottlenecking enzyme in bile acid metabolism of the classical pathway, which will produce up to 90% of all bile acids.
Now, if our liver put these bile acids together, they are then conjugated by amino acids, taurine & glycine, which we often lack in the modern food web. We call these conjugated primary bile acids.
They are then stored in our gallbladder and upon eating, CCK (a hormone) releases bile acids into the duodenum (the upper part of the small intestine). Main functions of bile acids are:
Uptake of Fats, Cholesterol and Vit ADEK
Antimicrobial Properties
Detoxification Agent
Influences Metabolism
Influences Thyroid Hormone Conversion
Impacts Gut Microbiome Composition
Immune Modulation
Insulin & Feeding Signaling

Within the gut, the metabolism of bile acids really starts. All bacteria contain bile modifying enzymes (like BSH, Dehydroxylases or Epimerases) which feed on certain bile acids and create “secondary bile acids”.
The small intestine is interesting in this regard as we got two things happening:
a) we generally have lower levels of bacteria (in normal states), so there are lower levels of secondary bile acids in this region
b) 90% of bile acids are taken up again before entering the colon, which are then re-used over & over again.
Within the colon, the remaining 10% are modified and then excreted.
In general, that’s BA metabolism. It gets interesting when the liver-bile axis breaks. Let’s look into that.
Pathophysiology of the liver-bile axis
If there is a weak link in metabolism over a prolonged period of time, inflammation kicks in. In the modern world, this is often a combination of:
subpar food choices
toxin accumulation
misaligned circadian rhythm
These will all impact the metabolism of this critical axis in some shape or form. Now, inflammation is directly linked to liver diseases like NAFLD & NASH (a side note: NASH is defined as NAFLD + inflammation. I do believe that inflammation had to be present for NAFLD to occur.)
Liver damage = disrupted bile metabolism
But what are the consequences? Here are some:
Toxin accumulation, as bile grabs onto fat soluble toxins and prevents them from re uptake before entering the colon. They are then excreted.
Bacterial overgrowths, as bile acids have antimicrobial properties. Low bile also pre disposes us to endotoxemia, a condition where gram negative bacteria produce toxins leading to severe inflammation, further enhancing liver damage.
Thyroid conversion is bile dependent. Low thyroid, as you will see, is important for gut motility & in general energy metabolism of any cell. This might lead to constipation, leading to toxin accumulation & overgrowths.
Last but not least, disrupted FXR & TGR5 signaling. These are the most important receptors bile influences.
In any of the above diseases, there is false expression of these receptors. They sit within the whole body, but mainly in the small intestine, colon, liver & adrenals.
To be honest, I could write two editions about these receptors, so I’ll give you a comprehensive rundown of their functions.
FXR & TGR5 regulate:
Glucose Homeostasis
Appetite & Feeding Behaviour (carb cravings!)
Microbiome Composition
Bile Acid Composition, Release & Production
Weight Gain (through GLP-1)
Lower Inflammation via immune modulation
Impact Thyroid Conversion (via DAO2)
Regulate Lipid Profile (ratio between HDL:LDL:TGs)
Energy Metabolism via uncoupling
Increases Glycogen Synthesis (interesting for athletes)
As you might notice, a breakdown of this signaling axis is pretty bad. And there are numerous studies showing disruptions of these pathways in diseases like obesity, diabetes, liver pathologies & gut diseases.
Now, let’s look into how to optimize bile.
How to optimize bile flow
First, I want you to ensure optimal intake of the following nutrients. Many people have suboptimal intake of these, so really hit numbers here:
Choline
Vitamin A/K
B-Vitamins (especially B1,B2,B3,B5)
Vitamin C (really important for CYP7A1)
Glycine
Taurine
Magnesium
In terms of bile, these are the most important and in general low within the population. Then, we want to optimize macronutrients & some meal decisions.
Conditions of low bile lead to bad absorption of fats. Often we have low bile as a root cause to SIBO & Co and normal dietary advise in these conditions might lead to high fat intake, which is inappropriate here.
Rule #1: Do not go keto or overly high on fat
Go moderately high until issues will resolve. Go for a balanced carb:protein:fat composition, adjusting carbs & fats to the state of your liver, bile, weight & fat levels.
Rule #2: Increase your intake of bitter foods
Bitter foods powerfully enhance liver & bile metabolism, so using these is a great way to improve many conditions. I am talking about artichokes, Swedish bitters, leafy greens & herbs. Do not overdo it, as these also contain oxalates, but in moderation these are great!
Cook the leafy greens in animal fats for a long time to counteract some of the effects that oxalates have.
A small trick, you can start your day with a small amount of coconut oil or EVOO, to stimulate bile. On an empty stomach in the morning, followed by a breakfast rich in egg yolks, some fruit & other condiments, this is a crazy good meal for liver & microbiome.
Last, but not least, we need to talk about circadian rhythm & optimizing sun exposure.
Vitamin D is very important, especially because of its actions on VDR in the liver. There it is important for everything metabolism: production, moving, re uptake & enzyme expression.
A normal circadian rhythm, by adhering to bright days (low ALAN) and dark nights will lead to proper entrainment of all organ systems, including the liver. The liver is then synched to the whole GI tract leading to optimal production of bile.
CYP450 enzymes are also controlled by light & dark cycles.
Cold thermogenesis also increases bile, so adhering to natural hot & cold cycles, adding in sauna & cold tubs weekly is also great!
Supplements I would consider are TUDCA & Ox Bile, which can be pretty helpful for many, but start with nutrients & lifestyle first. Choline might also be a valid option to supplement, if you suffer from neuroinflammation. Alpha GPC, Phosphatidylcholine or CDP Cholin are all valid here.
Thyroid: a missing link
This butterfly shaped hormonal gland is of utmost importance when it comes to everything related to metabolism & energy expenditure. Sadly, when our liver-bile axis breaks down, we will struggle with thyroid functioning.
Hashimoto’s is the most widely spread autoimmune disease, which is the equivalent to hypothyroidism with the added breakdown of thyroid tissue by immune cells. And this makes sense, if we consider that in all of these conditions the gut-liver axis has broken down.
Let me give you two reasons for this:

Look at this picture. This is a rough sketch of the lymphatic system in our neck region. You can see the thyroid glandular in the middle. Our lymphatic system is our immune system.
Our primary lymphatic organs, thymus & bone marrow is where our adaptive immune cells develop & proliferate. The secondary lymphatic organs, lymph nodes with its vessels, spleen & MALT are where these cells go to, circulate around and do their job.
The problem is that in todays society there is a massive pandemic of stuck & inflamed lymph floating around. The lymphatic vessel system is not like our blood circulation, driven by a pump, the heart. Our lymphatic system purely relies on mechanical forces, which drive fluid dynamics. It goes from point of high pressure to points of low pressure.
The most important “pumps” in this instance are movement, breathing and indirectly valves within the vessels. However it comes to no surprise to you that modern humans lack movement, have shallow mouth breathing with bad posture & have extracellular matrix (ECM) dysfunction, impacting not only the valves but also the “pipes” themselves.
Add excess, chronic inflammation which not only is a key driver of this ECM breakdown, but also a reason for overly high activation of our immune system over prolonged periods. The need for lymph circulation increases, while due to lifestyle adjustments, lymph flow is heavily disrupted.
Ever seen a highly inflamed person walk 10 000 steps a day? No, as the inflammation signals lying down as an energy conservation mechanism. These are just some reasons our lymph is stuck.
But what does this have to do with our thyroid? For that, we have to look at the brain-gut connection. The vagus nerve is the highway connecting our gut and brain. Via this nerve there is communication between the state of the gut & brain, signaling through various cytokines, neurotransmitters & metabolites deriving from the gut.
If the gut-liver-bile axis breaks down we inevitably will have inflammatory signals from our gut, via the vagus nerve, to the brain. This leads to neuroinflammation. Long term, this leads to a breakdown of the blood-brain area, essentially leading to something called a Leaky Brain.
It mimics Leaky Gut, but in the brain. As you might recall, if there is high inflammation we need our lymphatic system which is very expansive in the head & neck region. This acts as a drainage pipe for our whole brain, which every night clears the dirt & debris (old cells, proteins, ECM) via the glymphatic system.
On its way down, it bypasses the thyroid. Here is where the “magic” happens. Stuck lymph flow due to all the reasons we discussed leads to excess inflammation in an area close to the thyroid. There might be spillover of activated T & B Cells, which then falsely assume the thyroid is an enemy. Et voila, we got Hashimotos.
And I am not the only one thinking that this might be true. The doctor who found out about Hashimotos, Dr. Hakaru Hashimoto, first proposed the idea that this mysterious disease was due to pathologic states of the lymphatic system (his dissertation was called Struma lymphomatosa).

Another reason for the high incidence of thyroid impairment is the near fact that the thyroid has to be very sensitive to the state of our mitochondria. Our mitochondria are the sentinels between our environment & our internal body, as the state of energy production dictates the fate of the whole body.
As the thyroid is such a central organ to the whole energy metabolism, it has to be very adaptable, which is good, if we humans would live like our ancestors. Sadly, we don’t.
Whats the bridge to the liver-bile-axis?
As I told you inflammation via the gut will impact thyroid metabolism. This means we produce less T4 & T3, while also converting less T4 which is the inactive thyroid hormone. Due to signaling issues, we might also have desensitized thyroid receptors.
One reason for bad conversion is, apart from inflammation, impaired bile flow, due to bile signaling being essential for this conversion happening.
Low thyroid is also a key driver of constipation and slow gut motility, accelerating the onset of SIBO, endotoxemia or Leaky Gut.
Due to the impact the thyroid has on our lipid metabolism, there is a strong link between hypothyroidism & NAFLD. As thyroid hormone increases the expression of LDL receptors on hepatocytes, it generally lowers low density lipoproteins. The liver can use the cholesterol to build bile, while other organs can use it to produce steroid hormones.
HDL is also upregulated as apolipoprotein A1 (an important component of HDL) is increased. All in all, the thyroid then also controls the flux of endotoxins within our circulation, as HDL & LDL all are means of detoxification for these toxins stemming from the gut.
The thyroid cure
First, a very cautious notes: “Biohacking” your thyroid with exogenous hormones, high dosages of certain minerals & so on just mask the problem. In severe Hashimotos cases, there is the need for exogenous hormones, but otherwise, go the long term route first.
The biggest levers for thyroid functioning are simply controlling the toxic flux getting into & out of your body. This means healing your gut, excreting toxins & reestablishing homeostasis.
Nonetheless, there are many things you might do to support thyroid metabolism.
Diet & Nutrients
The most important nutrients for thyroid:
Iodine
Zinc
Selenium
All B-Vitamins
Choline
Magnesium
Vitamin A
Vitamin D
Potassium
Copper
Vitamin C & E
These are the most important. You generally hit those numbers if you eat an animal based blueprint, with some modifications. Them being, high intake of fish & seagrass for iodine, selenium & all other co-factors. Some amount of liver & organs, mainly for choline, copper & magnesium.
Doing adrenal cocktails is also extremely beneficial for the thyroid, but this is more of a band aid, as long as underlying root causes have not been dealt with. This means some source of whole food Vitamin C, a good sodium & potassium source and some magnesium.
A sensitive amount of carbs is also necessary in acute situations. Under low thyroid conditions there is also the high chance your body cannot use fats efficiently due to all the inflammation present. Some carbs, though not overly high, help to keep the thyroid firing.
Best sources are low glycemic fruits like kiwi or oranges and low amounts of potatoes or rice, depending on the severity of your gut issues.
UV light & cold are the most important nutrients
Starting of with UV light, I gotta admit that it might be the most important nutrient of them all.

As you can read from this study, it was found that UV light is highly protective of thyroid cancers. This is underpinned by the fact that black men had the worst survival rate. But why is that? Because their skin & biology is essentially primed for high UV light and the UK (where this study has been conducted) is not known for its high UV indices over the seasons.
We just found a mismatch between genetics & sun environment. Interestingly there is a clear cut indication that hypothyroidism is implicated in many melanomas (skin cancers), meaning that people with low thyroid have a higher chance of getting this.
Why is that? Melanoma cells express TSH receptors.
If there is high TSH (as in cases of low thyroid functioning) this leads to enhanced growth of these cells. It’s relatively simple. TSH is the stimulating hormone released by the pineal gland which then hits the thyroid and tells it to produce more thyroid hormone.
It is regulated by the amount of T3 & T4 present in the body. If there is low levels of mainly T3, we will increase TSH. Now read the following carefully:
UV light directly converts T4 into T3 in a process called photolysis (breaking by light). It was found that our skin is a major endocrine organ, so when UV light hits, T3 will be produced.
Now you also know why black people have higher incidences of thyroid cancers. Hypothyroidism is a risk factor for these types of cancers. Black people have more melanin in their skin, which is why the skin is darker.
It is there for a reason: to protect from massive amounts of UV light found in the origin regions of our species, the African continent. If you now live in the low UV UK, you will probably have zero UV light present to get the benefits of increased thyroid conversion.
Prescription: Get more UV light (safely)
Last but not least, you might also need the exact opposite: cold
Cold thermogenesis increases TRH, which is the hormone regulating TSH. The cold also sensitizes our hormone receptors to all hormones, meaning you need less for the same effect. You could be hypothyroid on paper, with no problems at all, due to this fact.
The cold also upregulates bile production, increasing the T4 conversion as mentioned earlier. It also wouldn’t surprise me if biophotons produced by the cold increase photolysis of T34 to T3, though there is no study on that.
I would advise you, after getting down the basics and calming an overreactive nervous system, to slowly introduce some cold into your weekly regimen.
Last but not least, I want to mention that lymphatic drainage around the neck is also a huge lever to pull. Doing neck massages, dry brushing & walking regularly is a great way to enhance lymph flow.
Now, this was it. It was a pretty long edition, but one I really enjoyed writing, as I try to optimize this axis even more.
If you want to get weekly protocols as such, feel free to add my newsletter to the mix here.
Hear you next week!